
The scope and focus of the eHealth infrastructure is different for each country. Some countries have focused on eGovernment[1] systems (e.g., national identification). Some have focused on UHC initiatives and have made investments in implementing the infrastructure necessary to support provider payments. For others, the focus is on directly supporting the care delivery network for primary care; this is the area where government and donor investments are being made.
Figure 10 illustrates a possible eHealth infrastructure design, generally reflective of the system architecture for OpenHIE,[2] a global open-source collaboration initiative that assists in the strengthening of national health information exchanges for the underserved.
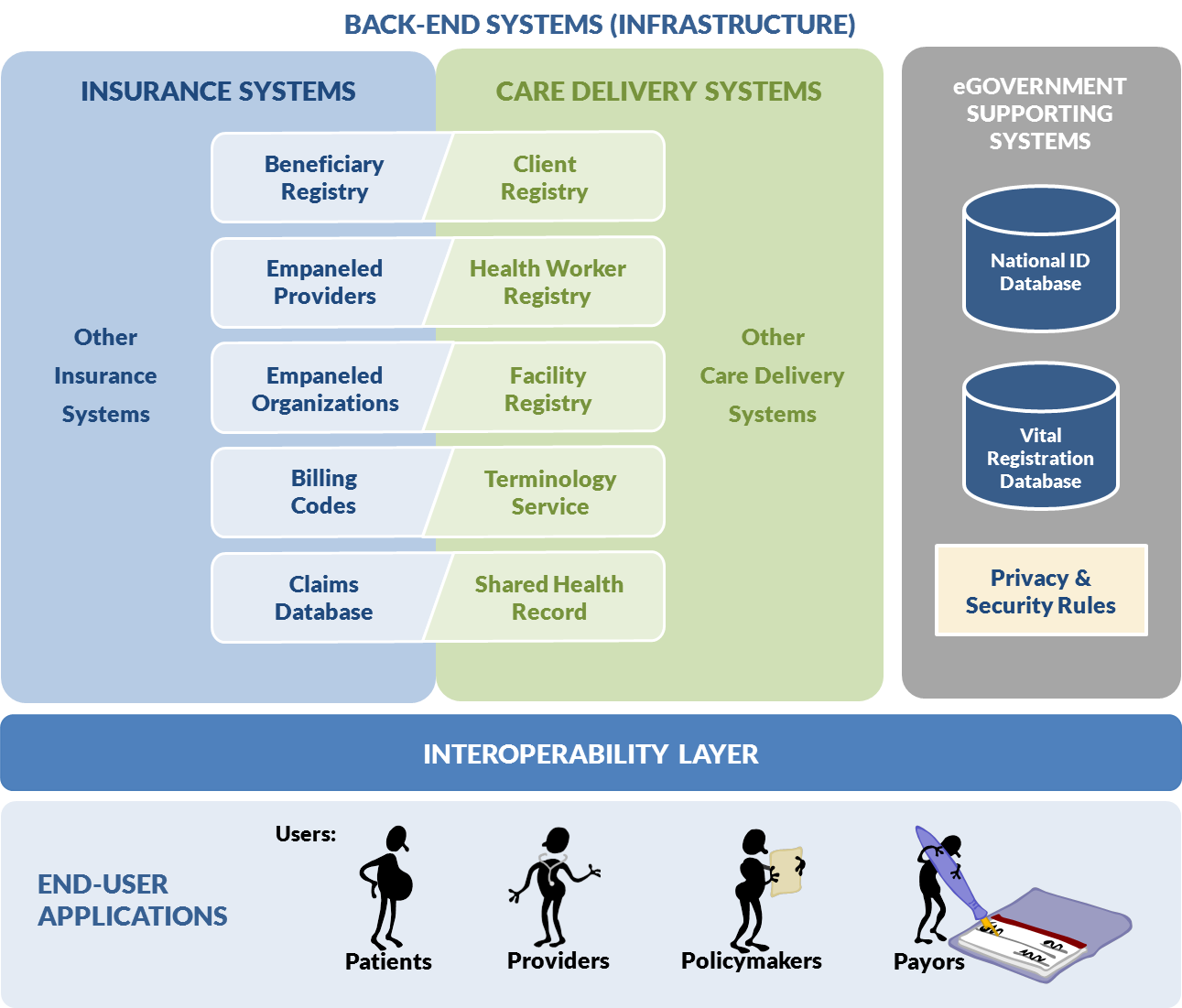
Figure 10 underscores a key message: reusable, standards-based eHealth infrastructure can and should be shared by the care delivery, insurance or payor, and “eGovernment” systems. Such shared infrastructure can then be leveraged by end-user applications that support transaction processing workflows and management analytics on behalf of patients, providers, payors, and policymakers. Data sharing topologies,[3] such as the interoperability layer-based design shown in Figure 10, can then be used to expose this shared infrastructure via standards-based “connectors” (application programming interfaces, or APIs). IT systems implemented on the insurance side can be leveraged by the care-delivery side; likewise, systems implemented to support care-delivery workflows can be leveraged to support provider payment transactions.
As an example, a country may have implemented a national facility registry (FR) to support specific care delivery initiatives (such as HIV, tuberculosis, or maternal care, for instance). At the most basic level, the “empaneled organizations” view of a facility registry provides sufficient information to support payments based on the global budget method. Using the global budget method, provider organizations are funded in advance of providing services based on their size, scope, and range of services. At higher levels of sophistication, adjustments might be applied to the global budget value based on factors such as service volume, services mix, or size of served population (catchment).
In contrast, if a country were implementing a UHC-focused insurance scheme that included a fee-for-service (FFS) payment method, more eHealth infrastructure would be needed. In FFS, individual providers (or sometimes, provider organizations) are funded, after delivery of care services, based on the services they have delivered. An empaneled provider (health worker) registry, a beneficiary (client) registry, and a claims database (shared health record) can be used to support FFS payments. Because the fee schedule is based on the specific services delivered, these billing codes must be part of the care service transaction record; a terminology server may be necessary to map between local and system-level codes (and enforce use of standardized codes, such as diagnosis codes based on ICD-10).
Regardless of which direction they are coming from (insurance to care delivery, or vice versa), a country’s eHealth infrastructure could be described using a capability maturity continuum and very simple descriptions for low, medium, and high (see Figure 11). Growing sophistication of the overall health care delivery and financing system will drive increased requirements for interoperability but will also provide increased value in the capabilities that can be derived from consistent connected data.
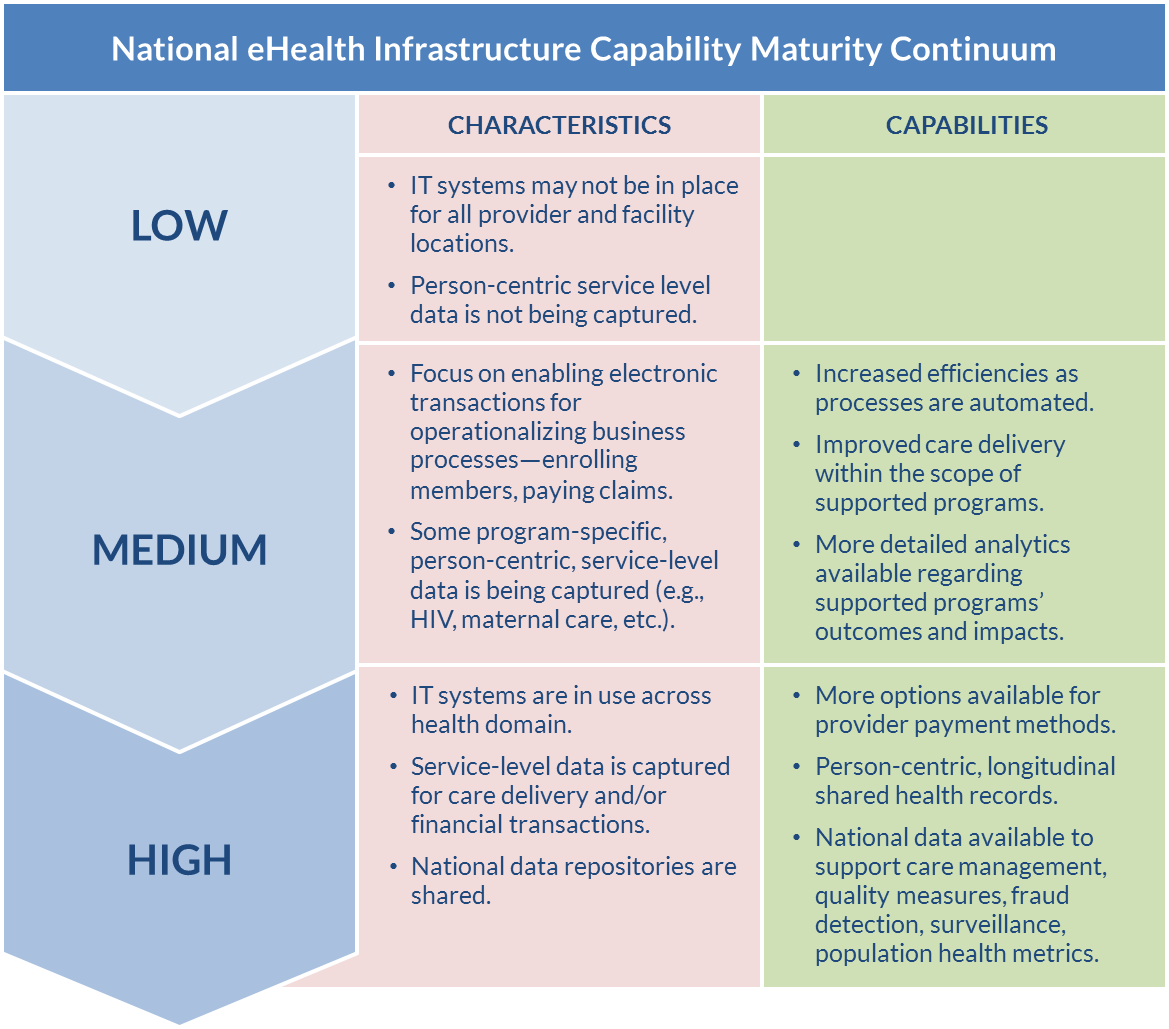
Wherever a country is starting on the continuum will define current requirements for interoperability. Equally important is the general recognition that countries will tend to move from low to high on the continuum, evolving toward greater levels of maturity. Greater maturity brings increased levels of complexity and increased needs for interoperability to support new capabilities and new demands for data.
Examples of drivers that cause a country to evolve its eHealth infrastructure include:
- Adoption of new technology and information systems.
- Patients paying premiums and being more invested in their health and the health services they receive.
- More sophisticated provider payment methodologies (e.g., performance-based financing) that require measuring quality and outcomes.
- Increased national demand for quality health care information to evaluate population health.
- Demand for measurements and evaluation of UHC reforms and progress, such as how much of the population is covered and enrolled, how equitable the coverage is, what services are covered, and at what cost are services covered.
What is the value of higher levels of maturity and interoperability? Information systems help to capture data in a standard format that enables them to be collected, reported on, analyzed, and used. Information systems also help to automate manual processes. Information systems can share information across or between systems so it can be collected, analyzed, and reported on across the broader health care system.
The following are examples of capabilities that can be enabled or supported by a national eHealth infrastructure that supports standards and interoperability:
- More options are available for provider payment methods. The capture of service-level data at the point of care and the standardization of service codes to be used for clinical care and for billing give the payor more options for using different provider payment methodologies. (See the paper Provider Payment Reform and Information Technology Systems: A Chicken and Egg Question for National Health Coverage Programs[4] for more information).
- The national use of shared health records would require standardized service-level coding and interoperability between point-of-care systems used by providers and facilities, national registries for patient identification and provider identification, and payors.
- Standardized data that can be collected and analyzed at a national level can be used to support population health metrics and feedback/input back to health policies.
- Billing data collected by payors can be used to evaluate potential fraud and abuse.
- National-level data can be used to support measurement and evaluation supporting UHC efforts, looking at how much of the population is covered, what services are covered, and at what cost services are covered.
- eGovernment refers to digital interactions between a government and its citizens. In the United Nations E-Government Survey 2012, it is defined as as “The employment of the Internet and the world-wide-web for delivering government information and services to the citizens.” ↵
- Page on OpenHIE’s Architecture. OpenHIE website. Available at: http://ohie.org/architecture/. ↵
- Data-sharing topologies can include options such as peer-to-peer, enterprise service bus (ESB), or hybrid network designs. ↵
- Provider Payment Reform and Information Technology Systems: A Chicken and Egg Question for National Health Coverage Programs. Wilson K, Latko B, Cashin C, Garabrant A, Hesp C, Stepney P, et al. The Joint Learning Network for Universal Health Coverage; 2013. Available at: http://jointlearningnetwork.org/uploads/files/resources/IT-PPM_FINALlores_online.pdf. ↵
