
Chapters 1 and 2 introduced the idea of eHealth infrastructure, explained why such infrastructure is important, and described the progress that has been made by selected countries toward establishing national-scale systems. This chapter introduces the four key actors who will provide information into and extract information from the eHealth infrastructure and the roles they play in relation to each other (see Figure 3).
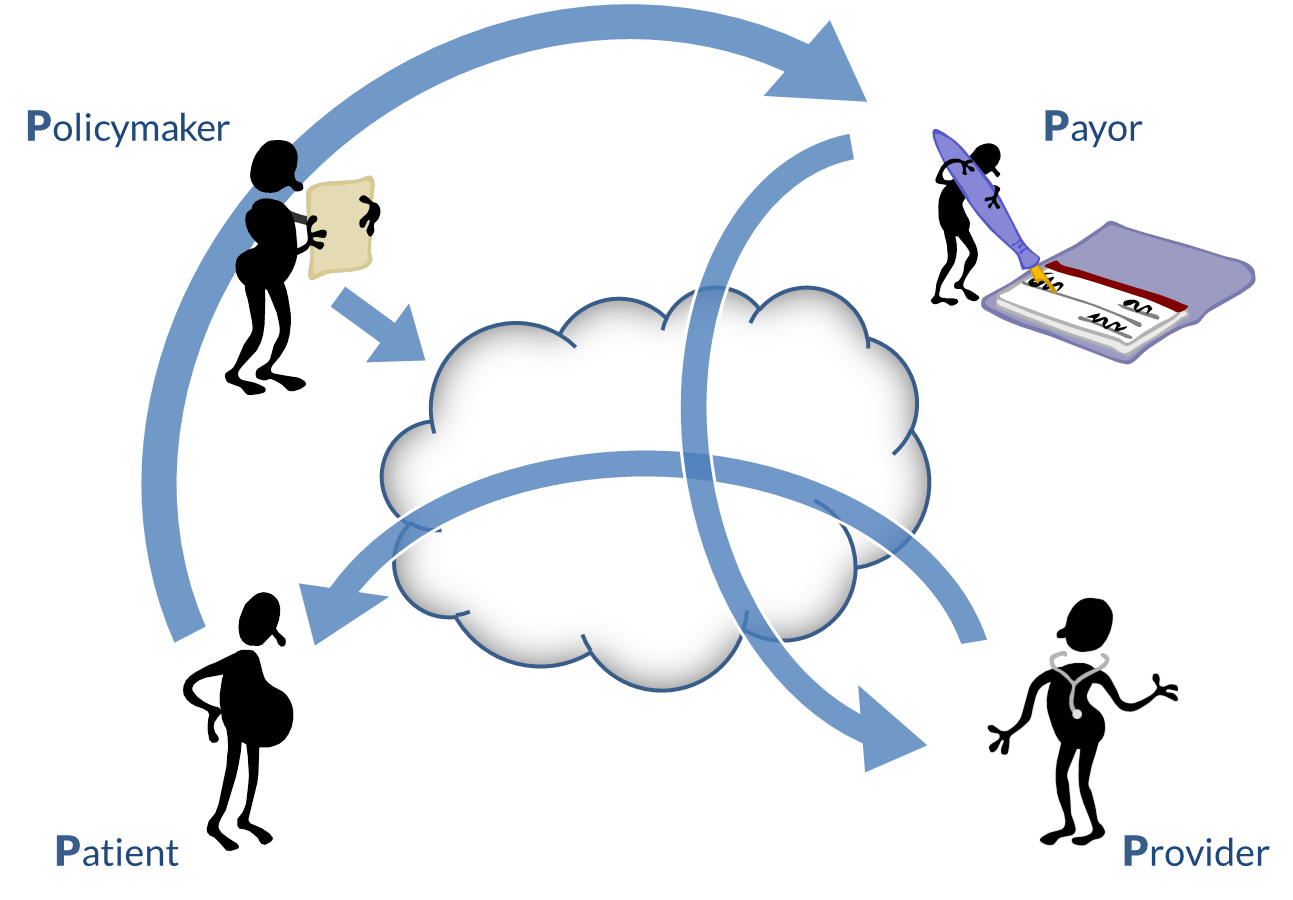
Developing a NeSF begins first by documenting a country’s representative health stories. We use health stories to denote common or characteristic healthcare scenarios expressed in a storytelling format. Here we look at four of the main characters in these stories:
- Policymakers. Policymakers establish the framework within which health care is provided to the country’s citizens. In this book, “policymaker” is a synonym for “ministry of health” or whatever jurisdictional entity is responsible for the health of the population. The policymakers aggregate data from patients, providers, and payors to develop population-level metrics that inform their health and health economic policies. In this context, policies answer the crucial questions:
- Who is eligible to receive care?
- What care services are provided; how; where; by whom?
- How are services paid for?
- Are the services being delivered well? Are they accessible?
- Are the needs of vulnerable or marginalized populations adequately served?
- What health care concerns do we need to plan for next?
- Patients. All of us—at one time or another—are patients. Patients are typically citizens, and voters, and sometimes taxpayers. Policymakers have a fiduciary duty to this population, and the country’s policy framework is established to benefit patients. Patients receive care services from providers and are the beneficiary customers of the payors. Patients also may want to access information about their care via an electronic device (e.g., personal computer, mobile phone).
- Providers. Providers operationalize care delivery within the policy framework. They provide health services to patients and maintain health information about them. The providers coordinate patient care with other providers as care team members. Many providers are independent businesses that must manage their own operations and finances.
- Payors. Payors operationalize the financial elements of the policy framework. Payors enroll patients as beneficiaries. They procure care services from the providers on behalf of their patient beneficiaries. They also must take on the actuarial task of ensuring the financial sustainability of the care program. They report to policymakers.
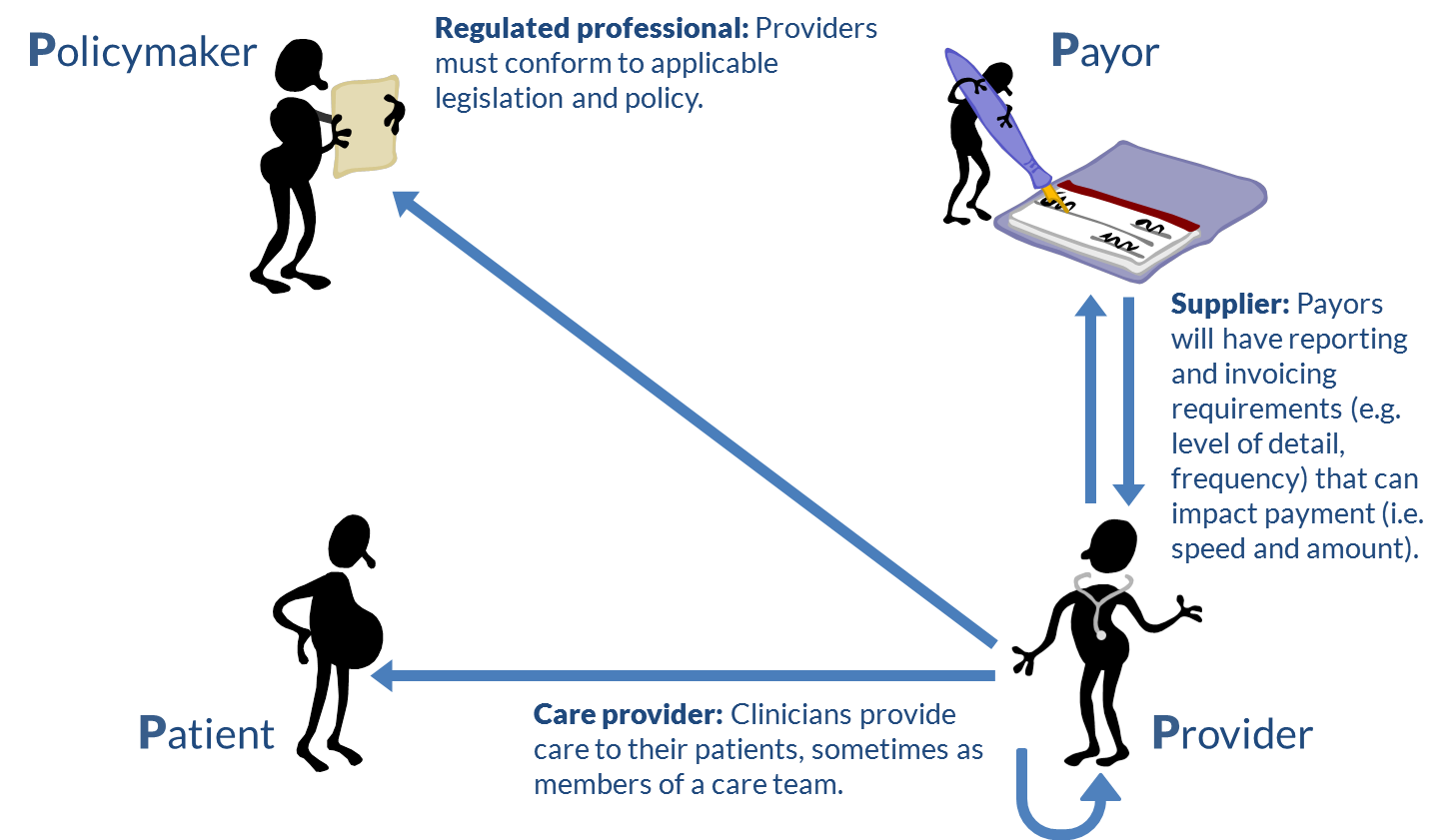
Each of these stakeholders plays a different role in relation to the others (Figure 4). Each has a different viewpoint on the health care value chain[1] and on the eHealth infrastructure needed to support it.
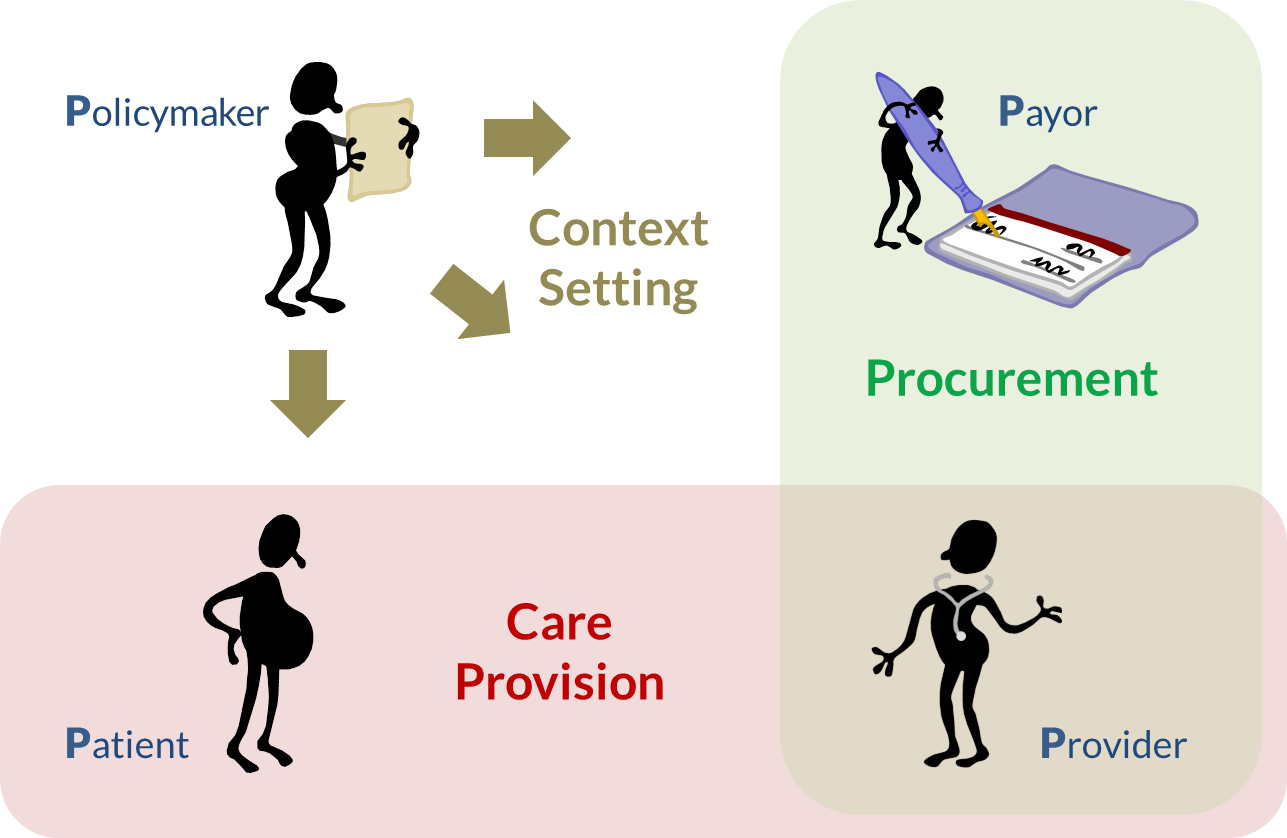
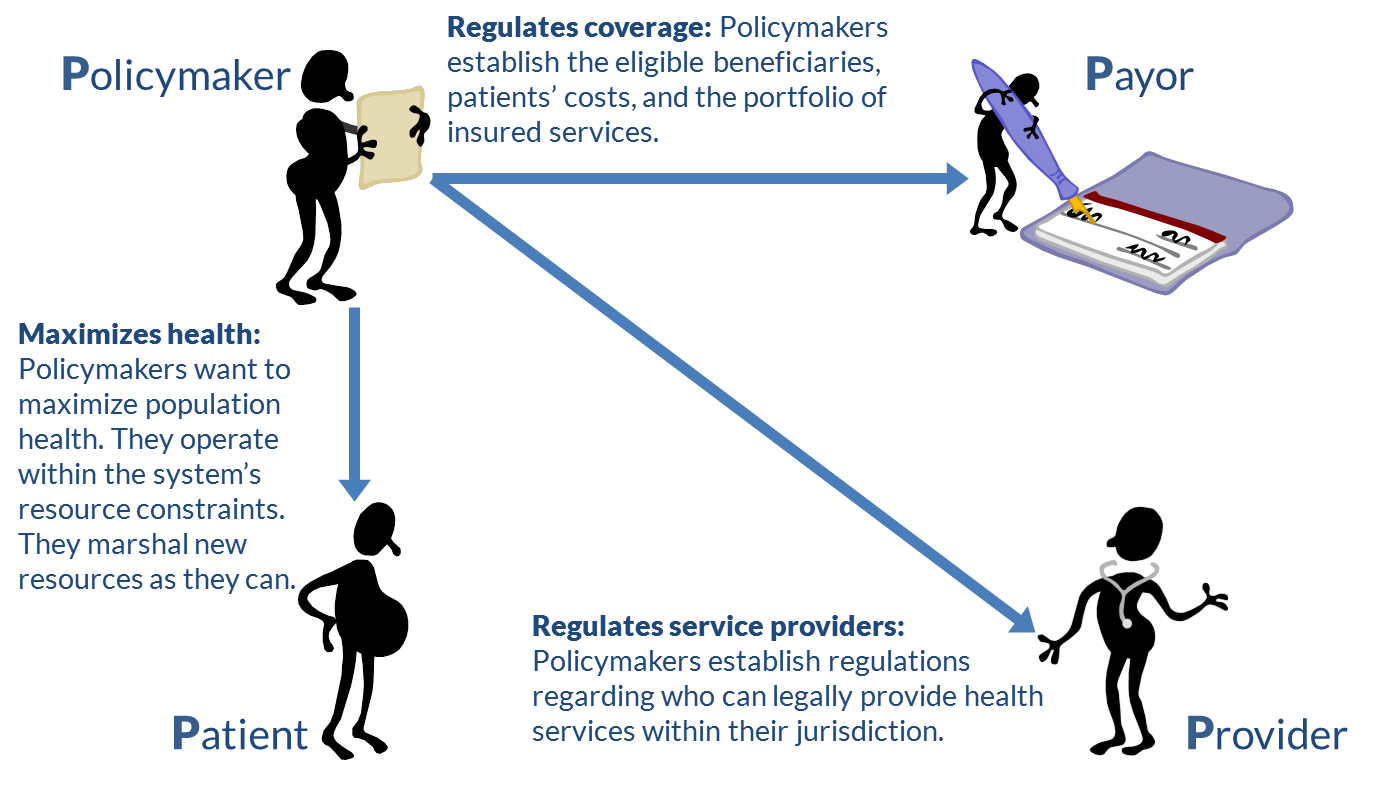
Policymakers set the context within which the health care system operates (Figure 5). Providers and payors are regulated by these policies and operate within them. Ideally, the policies are designed to maximize the health of the population within the country’s financial and resource constraints (recall the flows described in Figure 1).
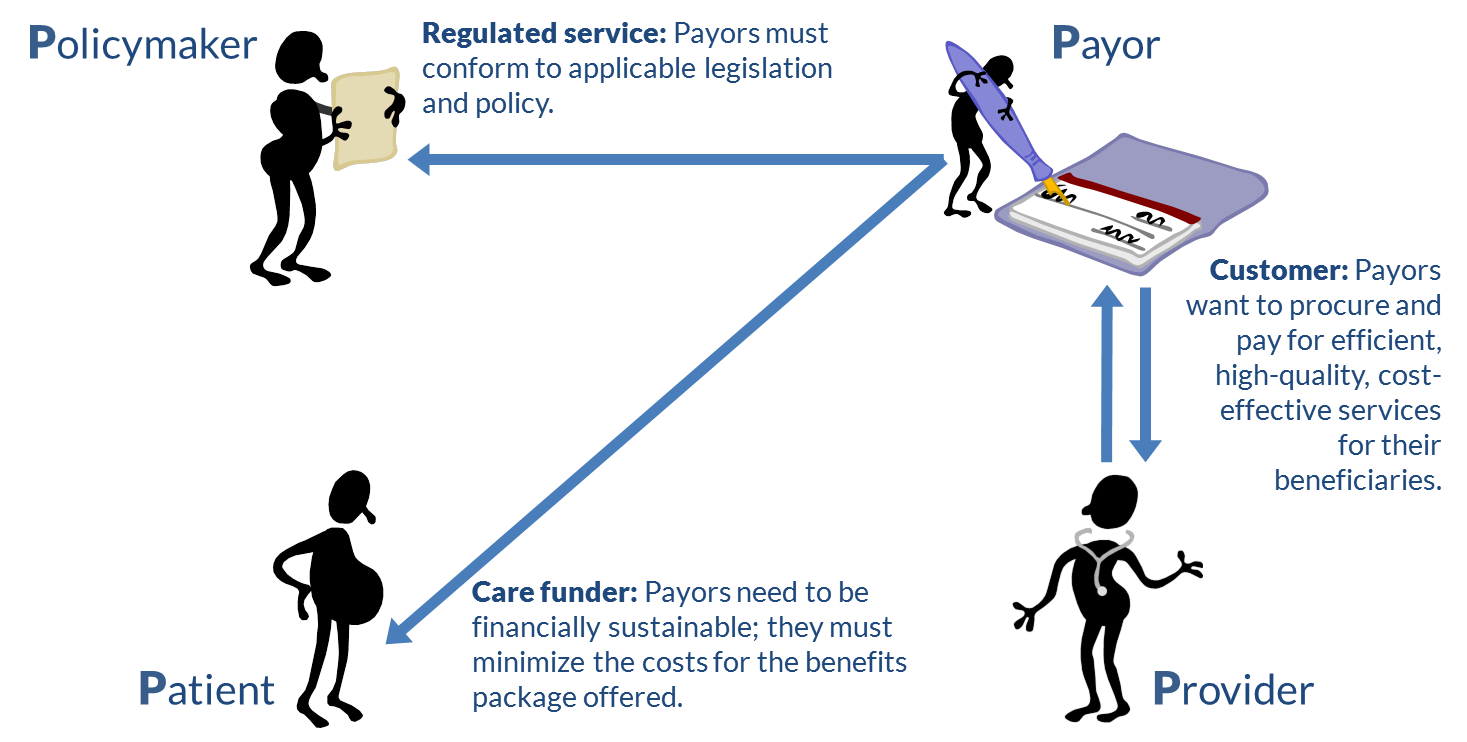
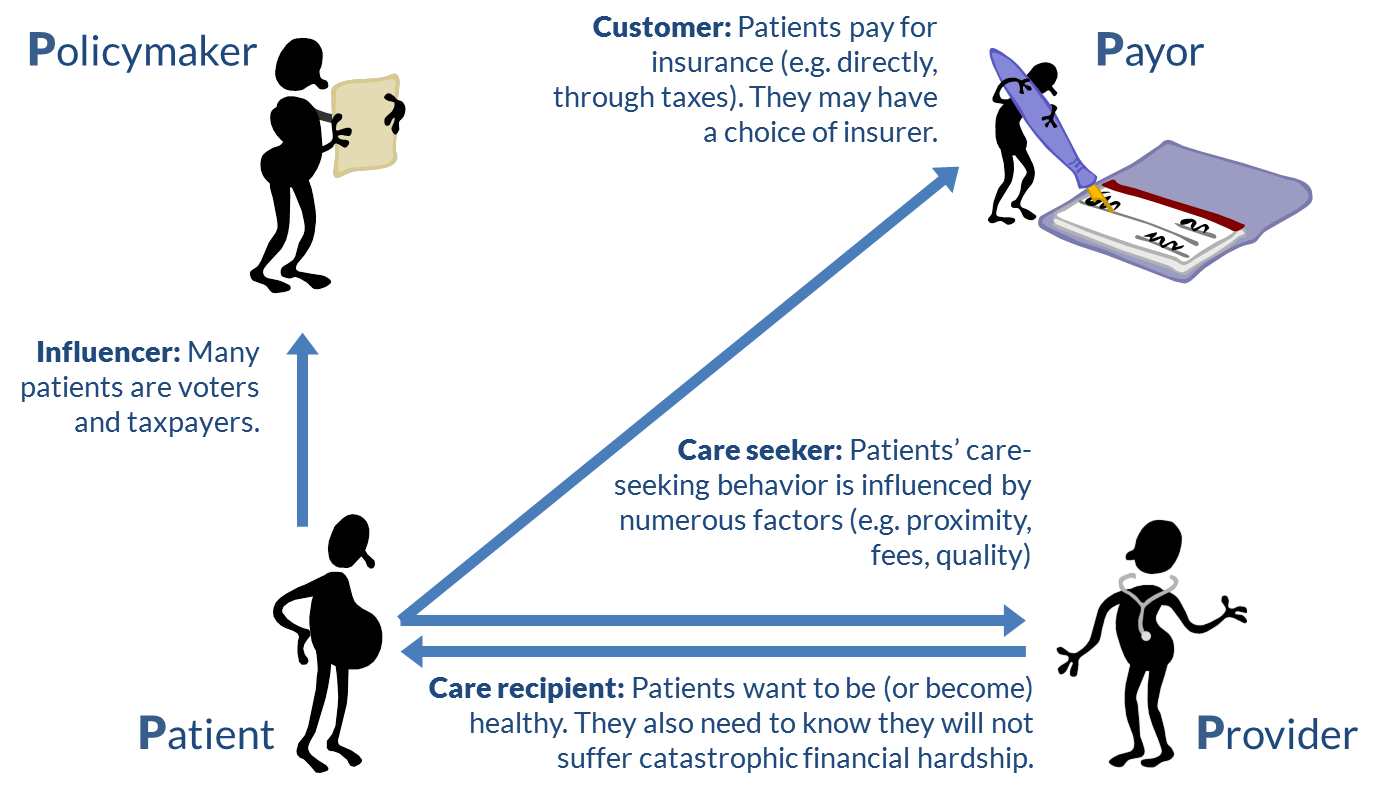
The payors’ view (Figure 6) is dominated by their role as procurers of services on behalf of their beneficiaries. In financial terms, payors and providers have a customer/supplier relationship. Of course, in turn, patients may have a choice of payors, and so payors may have a supplier/customer relationship with their patient beneficiaries. To be sustainable, payors endeavor to minimize the costs of funding their portfolios of care services. This incentivizes payors to encourage and even invest in the uptake of healthy-living initiatives within their beneficiary population.
The providers’ viewpoint (Figure 7) is defined by their care provision relationship with the patients and their supplier relationship with the payors. These relationships exist within the providers’ contextual relationship with policymakers as regulated professionals. In situations where care must be coordinated, providers also find themselves managing relationships with other members of the care team, as they collaborate on behalf of a shared patient.
The patient’s viewpoint (Figure 8), in times of good health, may be turned to their role as influencers of health policy (perhaps during an election). As consumers, patients may be able to exercise purchase discretion regarding their choice of payors. In times of poor health, patients are often powerless consumers. When we are ill, we want to become healthy again. This is what makes the patient-provider relationship powerful, and underlies the moral and ethical imperatives that are important to it.
How do these viewpoints relate to eHealth infrastructure supporting the operation of the health system? The different perspectives may be illustrated by looking at four common eHealth infrastructure elements (Figure 9):
- Patient database
- Facility database
- Provider database
- Health transactions database
The term patient database should be taken loosely; at any given moment, everyone is a potential patient. From the point of view of the policymaker, then, this all-person database is the client registry (CR)[2] and contains demographic information about all citizens, including information about each individual’s insurance plan and his or her preferred primary provider (PPP). From the payor’s viewpoint, the subset of the CR that references its customers constitutes a database of the payor’s beneficiaries. The subset of the CR that is related to a particular provider represents that provider’s patient list; for an individual patient, he or she thinks of the demographic record in the CR as a record about “me.”
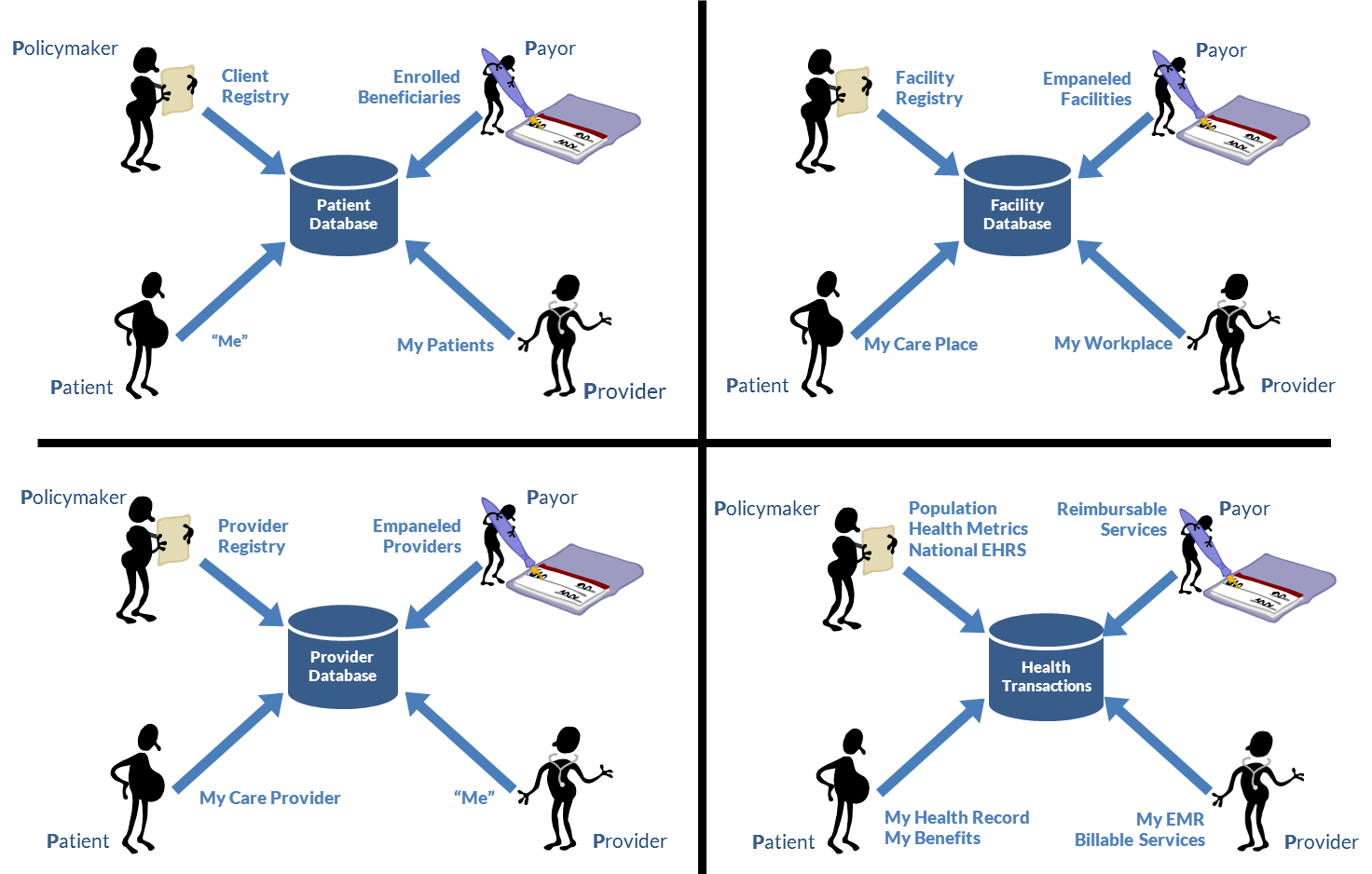
To the policymaker, a facility database represents the national facility registry or master facility list and is a tool for supporting health system management and planning. A subset of this national list, however, may have been empaneled[3] by the payor and would represent the payor’s list of authorized suppliers. To the provider, the facility registry includes the locations from which he or she delivers care. From the patient’s perspective, it is a provider database, listing the places where the patient receives or can receive care.
On a national basis, the policymaker views the provider database as the provider registry and uses it to support health human resource planning. For the payor, a subset of this list represents its empaneled list of suppliers. To an individual provider, his or her record in the provider registry is a demographic and professional record about “me.” From the patient’s prospective, this database contains current care providers and possibly a list of potential new providers.
It is interesting to consider the multiple viewpoints on the health transactions database. From the point of view of a policymaker, this database represents a national-scale electronic health records (EHR) system. Anonymized data from this EHR can be used to generate powerful analytics to inform health system management and planning, support disease surveillance, and generate public health metrics. From the payor’s viewpoint, this database contains an audit trail of reimbursable services. Likewise, for the provider, this is potentially a database of supporting documentation for the provider’s billings as well as an electronic medical record (EMR) for his or her patients. Of course, for the patient, this database represents the individual’s person-centric, longitudinal health record and, from an insurance standpoint, an audit log of his or her benefits.
A national eHealth infrastructure will contain ICT assets that serve multiple purposes. If these multiple viewpoints and purposes are understood during design, then these ICT assets can be deployed as shared assets rather than, inefficiently and expensively, as duplicative assets.
- Michael Porter, of the Harvard Business School, coined the term “value chain” to describe the entire production chain, from raw material and service inputs right up to final product or service ultimately consumed by the end user. For our purposes, the health care value chain includes the entirety of public health; preventive, primary, and acute care; and the management, supply chain, and financial systems that support these. ↵
- A client registry is sometimes also referred to as an Enterprise Master Patient Index (EMPI). ↵
- A payor establishes the criteria that must be met to be eligible for reimbursement as a service provider to its beneficiaries; the eligible services providers are said to be “empaneled” by the payor. ↵
